Virus Mimicry and Cancer Immunotherapy
Cancer Therapies Result in Formation or Accumulation of Aberrant DNA and RNA in the Cytoplasm
Cancer cells encounter aberrant nucleic acids not only in the tumor microenvironment but also as a result of common cancer therapies such as radiation and chemotherapy. This is because genotoxic therapies can generate micronuclei, which are abnormal DNA structures that are produced as a consequence of the DNA damage response. Other types of DNA that can accumulate in the cytoplasm after damage include DNA from mitochondria. Besides DNA, genotoxic insult can also lead to the de-repression of certain non-coding RNAs (e.g., ERVs, retroelements), which have viral origins and are widespread in the genome. Normally these viral-like RNAs are transcriptionally silent; however, after DNA damage or other cellular stress, these RNAs can become transcriptionally active again. In all of these situations, the DNA/RNA finds itself in cellular compartments where it does not normally belong.
Cancer cells before and after irradiation. After radiation, micronuclei are generated and retroelements are de-repressed.
Genotoxic Cancer Therapies Can Result in Virus Mimicry and Activate an Anti-Viral Response
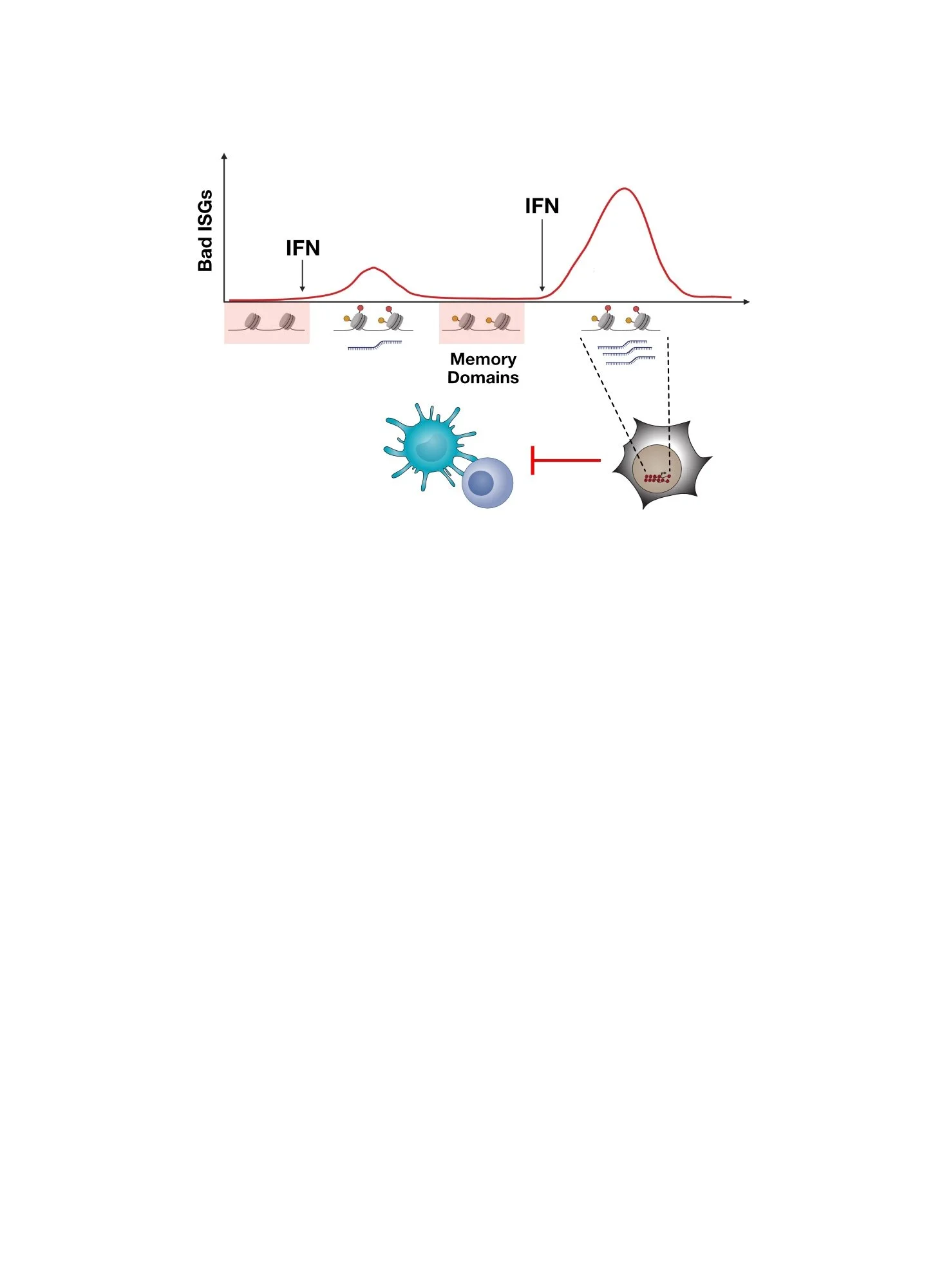
What happens when DNA and RNA generated after cancer therapies accumulate in wrong places? Just like after infection by a virus, these nucleic acids activate DNA and/or RNA pattern recognition receptors (PRRs). Micronuclei can be recognized by the DNA sensor cGAS, as demonstrated by studies led by our collaborator Roger Greenberg, while aberrant RNA can engage PRRs such as RIG-I or MDA5. PRR activation results in production of interferon (IFN) and the induction of IFN-stimulated genes (ISGs). Since infection with a virus typically activates the immune system, do cancer therapies that lead to an anti-viral response also put the immune system on high alert?
Depiction of how endogenous DNA (e.g., micronuclei) and endogenous RNA (e.g., retroelements) can activation pattern recognition receptors like viruses do, resulting in interferon and interferon-stimulated genes.
Activation of an Anti-Viral Response by Cancer Therapies Can Improve Immune Function
Interferons have important functions in enhancing the immune response. This includes the role of type two IFN (IFNG) in promoting antigen processing and recognition by T cells (antigenicity), and the role of type one IFN (IFN-I) in helping innate immune cells, such as dendritic cells, facilitate T cell activation and hence expansion (adjuvanticity). Thus, if genotoxic cancer therapies like radiation can enhance PRR and IFN signaling, are these therapies immune stimulatory? If they are, can they be used to improve the efficacy of immunotherapies like immune checkpoint blockade, which include anti-PD1/PDL1 and anti-CTLA4?
Immune functions improved by genotoxic therapies include better antigen processing and recognition (antigenicity) and better engagement of innate immune cells to facilitate T cell function (adjuvanticity). Both of these are heavily influenced IFN-I and IFNG.
Radiation Improves T Cell Function Even in Unirradiated Tumors
When cancer patients are treated with radiation, very rarely response can be seen not only in the irradiated tumor but also in unirradiated, or abscopal, tumors as well. Case reports of these rare abscopal effects were speculated to result from radiation somehow affecting the immune system. With evidence that radiation can activate an anti-viral response, the potential for an immune-mediated abscopal effect makes a lot more sense. Indeed, when tested in mice using single-cell technologies, radiation therapy can cause T cells in unirradiated tumors to expand. When immunotherapies such as immune checkpoint blockade are added to radiation, these T cells also further expand in the blood. These expanded T cells seemingly have undergone antigen-driven selection that is unique to the addition of radiation, as indicated by distinct amino acid properties found in the T cell receptors (TCRs) that make contact with antigen and MHC. Thus, recent experiments like these have rekindled interest in the abscopal effect, a historically rare clinical observation and subject of medical case reports. With the availability of immunotherapies like immune checkpoint blockade, can such rare occurrences be routinely elicited to help treat cancer?
After tumor irradiation, T cells in unirradiated tumors expand. Upon addition of immune checkpoint blockade (e.g., anti-CTLA4 and anti-PDL1), some of these T cells additionally expand in the peripheral blood. These expanded T cells have distinct T cell receptor (TCR) properties, suggesting antigen-driven selection.
Radiation Can Improve The Efficacy of Immune Checkpoint Blockade
Given the ability of radiation to work together with immune checkpoint blockade to expand T cells and impact the TCR repertoire, can this combination also improve tumor response? In mouse models of cancer, response from radiation plus immune checkpoint blockade is better than response observed from the individual therapies. Currently, many clinical investigations across a variety of different cancer types are underway to formally demonstrate that better responses can result from this one-two punch in patients. Although it is too early to draw conclusions, there is emerging evidence that the addition of radiation might improve the efficacy of immune checkpoint blockade in certain scenarios.
However, despite evidence in mice and potential signals in humans, resistance and relapse even to such combination approaches are nonetheless frequent. How does resistance and relapse after cancer immunotherapy develop? Can this somehow be related to virus mimicry as well? Find out here.
Improved survival in mice bearing melanoma tumors after radiation plus anti-CTLA4. Response of unirradiated (abscopal) tumors when radiation is used with immune checkpoint blockade (e.g., anti-PD1) can be observed in patients as well.
Listen to the story of a patient treated with anti-CTLA4 and radiation at UPenn that inspired our research.
The full story by WHYY public radio can be found HERE.
Interested in reading more?
Visit our publications page to find the full references for our work and collaborative work led by our colleague Roger Greenberg.
Twyman-Saint Victor et al, Nature 2015
Harding et al, Nature 2017
Here Are Some of the People That Led The Studies and Made It Happen!
Tina Twyman-Saint Victor, former research fellow
Andrew Rech, former grad student in Bob Vonderheide’s lab
Shane Harding, former post-doc in Roger Greenberg’s lab
Joseph Benci, former grad student and post-doc